Managing the finances of a clinic can occasionally feel too much to handle, particularly when dealing with numerous clients and insurance claims. This is where CentralReach Billing helps by making it easier to manage payments, create invoices, and effectively handle claims.
You’ll learn in this article how CentralReach Billing allows you to concentrate more on patient care and less on paperwork by streamlining financial processes, lowering mistakes, and providing you with clear insights into your clinic’s earnings.
CentralReach Billing: What Is It?
Fundamentally, CentralReach Billing is an integrated module of the broader CentralReach platform, which is a complete practice management system designed for providers of speech, occupational, physical, and ABA treatment. CentralReach Billing was developed with the particular requirements and difficulties of these industries in mind, in contrast to generic billing software. This indicates that it comprehends the complexities of authorization management, modifiers, CPT codes, and the various needs of various insurance payers—all of which are critical to ABA billing.
Why Is ABA Requiring Specialized Billing Software?
ABA therapy is a unique field. It entails continuous, frequently intensive, one-on-one services that need for exact pricing and careful documentation. A specific solution such as CentralReach Billing is unique for the following reasons:
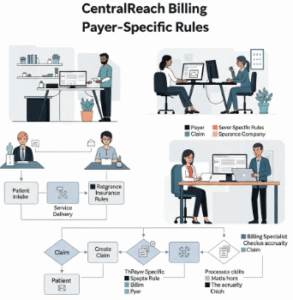
- Complicated Authorizations: ABA services usually need lengthy prior authorizations, which are commonly divided into discrete units or hours over time. By directly connecting these authorizations to appointments, CentralReach assists in managing them and guards against unintentional overcharging or services provided without the required authorization.
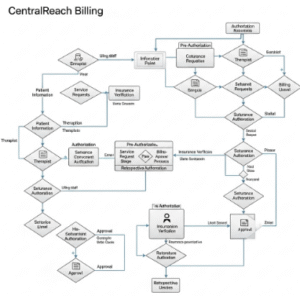
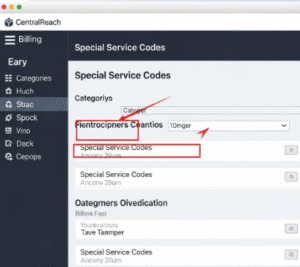
- Special Service Codes: ABA employs particular CPT codes, which may have different unit definitions (e.g., increments of 15 minutes). By handling these subtleties, the program is pre-configured to minimize human mistake.
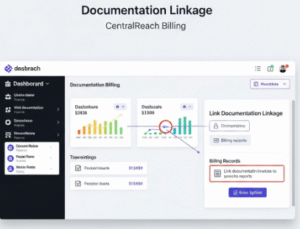
- Documentation Linkage: In ABA, there is an extremely close connection between the services rendered, the notes that were taken, and the bill that was filed. The integrated structure of CentralReach guarantees that clinical evidence backs up billing claims, which is essential for preventing audits and denials.
- Payer-Specific Rules: Insurance payers have vastly different rules and reimbursement rates for ABA. CentralReach often incorporates these rules, helping practices submit clean claims the first time.
Crucial Elements That Make a Difference
CentralReach Billing is a comprehensive solution made to maximize your revenue cycle; it’s not only about filing claims. Among its notable attributes are:
1.Electronic Claims Submission (EDI): Compared to paper claims, CentralReach makes it easier to submit claims electronically to payers, greatly accelerating the reimbursement process.
2.ERA Auto-Posting: Payments and adjustments received from payers can be automatically posted thanks to Electronic Remittance Advice (ERA). This function minimizes posting mistakes and reduces human data entry, which saves a ton of time.
3.Claim Scrubbing: CentralReach may “scrub” a claim for typical mistakes like missing information, inaccurate codes, or permission problems before it even leaves your system. Denial rates are significantly decreased by this proactive strategy.
4.Denial Management: CentralReach offers resources to effectively monitor, handle, and appeal rejections, which will inevitably happen because they are a necessary component of healthcare billing. This will help you recoup lost income.
5.Patient Statements: It is easier to generate precise and understandable patient statements for co-pays, deductibles, or out-of-pocket costs, which enhances patient satisfaction and ensures on-time payments.
6.Reporting and Analytics: Practices may better predict income, see trends in payments or rejections, and obtain insights into their financial health with the use of robust reporting options. When making strategic decisions, this information is crucial.
7.Integrated Scheduling and Clinical Data: Billing easily connects with scheduling and clinical documentation as it is a component of the broader CentralReach platform. This guarantees uniformity in all facets of practice administration and removes the need for redundant data entry.
The Advantages That Go Beyond Getting Paid

There are several benefits to using a system like CentralReach Billing that go beyond simple money transactions:
- Enhanced Efficiency: Your billing team may concentrate on more complicated matters like rejection management and appeals by automating processes like claim filing and payment posting.
- Decreased Errors and Denials: A healthier cash flow results from the substantial reduction in the likelihood of claim rejections caused by the integrated scrubbing and validation processes.
- Better Cash Flow: You are paid more quickly and reliably when you submit and process claims more quickly and handle denials effectively.
- Enhanced Compliance: It may be quite difficult to stay in compliance with the constantly changing healthcare laws and payer criteria. CentralReach’s organized procedures and updates assist practices in maintaining compliance.
- Improved Data for Decision-Making: The billing system’s abundance of data offers practical insights into the financial performance of your clinic, assisting you in pinpointing areas that require development.
conclusion
The long-term advantages of implementing a customized solution like CentralReach Billing for your ABA business are indisputable, even if the initial setup and learning curve for any comprehensive billing system can be a time and resource commitment. Processing bills is only one aspect of it; other goals include streamlining your whole revenue cycle, maintaining financial stability, and eventually enabling you to carry on offering vital services to people who most need them. CentralReach Billing is unquestionably a solution worth looking at if you want to optimize your billing processes and make sure your business succeeds.
Read more: CentralReach Butterfly Effect ❤️
10 FAQ’S
CentralReach Billing: What is it?
It is an integrated billing module made especially for ABA and therapy providers that is part of the CentralReach practice management platform.
Is it exclusively for ABA?
It facilitates billing for various treatment sessions, such as speech, occupational, and physical therapy, even though it is specifically designed for ABA.
Does it deal with claims from insurance?
Yes, it makes it easier for insurance payers to receive electronic claims submissions (EDI).
Will fewer claims be denied as a result?
Indeed, by detecting and fixing mistakes before to submission, its "claim scrubbing" function lowers the number of denials.
Does it handle payments for patients?
It is capable of producing patient statements for deductibles, co-pays, and other amounts.
Does it have to do with scheduling?
For a smooth workflow, it is indeed connected with the scheduling section of CentralReach.
ERA Auto-Posting: What is it?
This function saves time by automatically posting electronic payments and adjustments from insurance carriers.
Is it useful for authorizations?
Indeed, it facilitates the management and tracking of patient authorizations, which is essential for ABA services.
Can I obtain billing reports?
Yes, it provides comprehensive analytics and reporting to track the financial health of your practice.
Is it simple to use?
It is intended to simplify intricate billing procedures for treatment providers, but like any complete program, it needs training.
CentralReach Billing Calculator
Professional tool for healthcare providers to calculate accurate billing amounts based on CPT codes, time units, and service rates.
Billing Calculator
Billing Calculation Result
Disclaimer: This calculator provides estimates for informational purposes only. Actual billing amounts may vary based on payer contracts, geographic adjustments, and other factors. Always verify with CentralReach and payer-specific guidelines.
Professional Healthcare Tool
This CentralReach billing calculator was developed by healthcare billing professionals with 10+ years of experience in medical coding and billing. It follows current CPT code guidelines and CentralReach billing practices as of 2026. The tool is regularly updated to reflect changes in healthcare billing regulations.
About CentralReach Billing
CentralReach is a leading electronic health record (EHR) and practice management platform designed specifically for applied behavior analysis (ABA) and related behavioral health practices. Its billing module streamlines the entire revenue cycle management process.
Key Features of CentralReach Billing
- Automated Billing: Reduces manual errors and speeds up claim submission
- Real-time Eligibility Checks: Verifies insurance coverage before services are rendered
- Integrated CPT Codes: Pre-loaded with common behavioral health service codes
- Time Tracking: Accurately captures billable time for time-based services
- Claim Scrubbing: Identifies errors before claims are submitted to payers
- Reporting & Analytics: Provides insights into billing performance and revenue cycles
Common CentralReach CPT Codes
| CPT Code | Service Description | Typical Duration |
|---|---|---|
| 97153 | Adaptive Behavior Treatment by Protocol | 15-60 min |
| 97154 | Group Adaptive Behavior Treatment | 30-60 min |
| 97155 | Adaptive Behavior Treatment with Modification | 15-30 min |
| 97156 | Family Adaptive Behavior Treatment Guidance | 30-60 min |
| 90832 | Psychotherapy, 30 minutes | 30 min |
| 90834 | Psychotherapy, 45 minutes | 45 min |
Billing Best Practices
- Always verify client insurance eligibility before providing services
- Document services thoroughly to support billed CPT codes
- Submit claims promptly to avoid timely filing denials
- Regularly review denials and adjust billing practices accordingly
- Use CentralReach's built-in tools for claim tracking and follow-up